FALLS CHURCH, Vir. — It was Oct. 11 when the 38th surgeon general of the Navy rose from his chair to greet Navy Times.
An aide announced that their visas had gone through, so Vice Adm. C. Forrest Faison III would jet to Brazil hours later to deliver a keynote speech on the Navy’s experience with what’s called “value-based care.”
In São Paulo, physicians from across the hemisphere lauded Faison’s Navy Bureau of Medicine and Surgery for ongoing efforts to improve the treatment of sailors and Marines, military retirees and their families in an era of skyrocketing healthcare costs.
“We’re going through the most substantive and transformative changes in healthcare in 50 years,” Faison told Navy Times.
He retired two weeks later. He’s been replaced by Rear Adm. Bruce Gillingham, an orthopedic surgeon, who was confirmed on Halloween by the Senate.
Faison touched on the medical innovations that made his address in Brazil possible, plus the partial installation of the Defense Department’s $4.3 billion electronic health record system – MHS GENESIS – at Naval Hospital Bremerton and Naval Health Clinic Oak Harbor in Washington and how he almost became a preacher instead of a neurodevelopmental pediatrician.
But much of the hour was spent remembering the war in Iraq.

He spoke of the large number of patients who arrived at his field hospital with limbs lopped off by improvised explosive devices. He paused, then recalled the morning after a green medical crew arrived, the three helicopters rising over the horizon, nine IED casualties inside, several of them amputated by blast and steel, one patient dead on arrival.
They began triage on the tarmac.
“Blood everywhere. And there, right in the middle of all this carnage, was a young hospitalman apprentice, about 19 years old, from the clinic in Gulfport, Mississippi, where the only thing he’d ever seen was a runny nose, standing there in shock. About the color of the white in that paper,” Faison said, pointing to a nearby notepad.
“I went over to him and I put my arm around this young man and I said, ‘How’s it going, son?’
“‘Uhhh. OK.’”
“I said, ‘Tell me about your home.’ Over the next 10 minutes or so, I talked him out of shock, so he could go back and be part of the resuscitation effort. But we can’t do that for every corpsman. People will die. So corpsmen have got to see blood. They must become comfortable around trauma.”
After he took the helm of BUMED four years ago, Faison’s urgent mission became convincing a sprawling bureaucracy to prepare for what could be a much uglier war waged against a rising rival, like China.
In the halls of the Pentagon, White House and Capitol Hill, however, a very different war has occupied much of his time, an ongoing battle to contain healthcare costs and a series of spending bills over the past three years designed to reorganize military medicine to dig for deeper savings.
That was punctuated in President Donald J. Trump’s Fiscal Year 2020 budget request to Congress and its plan to trim about 18,000 medical billets from the Air Force, Army and Navy, which also provides healthcare for Marines and their families.
Pentagon officials estimate a quarter of the slots are empty already and some uniformed positions can morph into civilian jobs increasingly overseen by the Defense Health Agency, which was launched in 2012 to better integrate the services’ military treatment facilities dotting the globe.
That’s why Faison met Navy Times inside DHA’s Falls Church headquarters. His office was there, too.

What the proposed budget cuts and ongoing mergers mean for the Navy’s clinics, hospital ships and research units around the world is unclear, but the figure that glows like neon in Faison’s brain is “5,386.”
That’s the number of medical personnel he might need to boot to satisfy budget cuts. At the same time, the Pentagon is trying to build a 355-ship Navy and expand the sea service’s air squadrons, commands that will need more medical personnel to staff them.
If enacted, the sailors most likely to be affected are the 30,000 active duty corpsmen. They’re divided into 40 technical specialties, everything from the dental lab to urology, and corpsmen serve at 128 different facilities across the globe and on board ships at sea. They’re taking care of 2.7 million people.
“This is personal to me because I ran a combat hospital in OIF,” said Faison. “And I looked in the eyes of those casualties as they were offloaded from the helicopters. They’re missing an arm. They’re missing a leg. I look in their eyes and I see the fear. And I see that we made a commitment to you.
“I talk to Navy Medicine and I tell them, ‘Look, we’re honored to take care of the less than 1 percent of our nation that will sacrifice to serve and defend our freedom. And every single one of them is depending on us to provide them the best care our nation can offer and to do everything in our power to return them home to their families, safe and alive. I consider that to be a trust and that trust is put into our hands every day.’
“When I look in their eyes, I see them asking, ‘You’re going to make good on that trust for me, aren’t you, Doc?’ That’s why I look at the system and all these changes and say, ‘We have to make sure that no matter what we do in the future, we have to make good on that trust.’”
Officials at the Pentagon and DHA declined to talk to Navy Times about the proposed cuts or Faison’s fears, except to note that House lawmakers inserted language into a rival spending bill that would postpone many of the changes until the Pentagon produces detailed plans that account for risks to beneficiaries, especially service members prepping for future combat.
“I’d be very, very clear, and define in very fine detail, this question for reform: ‘What is success? And what does success look like?’” he said. “As you start to make changes to this health system, you ought to have a pretty clear definition and understanding about what success is.
“There are those who would say that ‘success is an integrated system of readiness and health.’ But what does that mean? Every service member and their mom and dad back home is depending on that system to deliver the same combat survival rate in any future conflict.”

Faison warns that the Navy isn’t “Kaiser in uniform,” a nod to the massive California-based managed care consortium Kaiser Permanente, a health network that generated nearly $80 billion in revenues last year and treated more than 12 million patients.
About 28 percent of Faison’s staff exited the service this year – 14 times higher than the typical turnover rate at a civilian hospital. And they’re young. Nearly 40 percent of BUMED’s workforce graduated from high school less than five years ago.
The Navy relies on that all-volunteer force, and too many cuts could ripple through a civilian population he needs for talent, sending the message that the military isn’t hiring.
Faison also cautioned that his medical system is “matrixed.” For example, a baby delivery room needs a galley, or moms don’t eat. His entire healthcare system functions in the same way, with key parts supporting others in ways outsiders often don’t notice.
“It’s all connected,” Faison said. “Because of that, as you start to make cuts and changes there isn’t a linear relationship between cuts and impacts. Because it’s so matrixed, you actually reach a tipping point, beyond which the system starts to collapse. You ought to know what that tipping point is.”
During the wars in Afghanistan and Iraq, Navy Medicine guaranteed a 97 percent battlefield survival rate for wounded troops, an unprecedented accomplishment in American military history.
Several key factors helped make that possible, including American air superiority and an abundance of aircraft to ferry casualties quickly to trauma centers strategically placed around the countryside because U.S. forces seized and held the terrain. A seamless communications network connected casualties and their caregivers from the point of injury to a hospital back home.
A rival power such as China or Russia could take those advantages away, and how the Navy organizes for combat at sea doesn’t help.
The focus for generations was the Navy’s large hospital ships. But as the fleet began to embrace concepts such as “distributed lethality,” spreading vessels across vast distances to survive enemy detection and ship-killing weapons, the floating trauma wards lost relevance.
War games convinced Faison that the Navy must staff destroyers with surgical teams able to supplement the vessels’ medical departments. And those teams need seasoned corpsmen who won’t flinch at the first sight of blood.
They also needed to learn how to stretch the “Golden Hour” of lifesaving into what likely will be hours, even days, of constant care as patients are transported across long distances to a hospital ship or clinics ashore.

Because the wars in Iraq and Afghanistan waned, Navy hospitals don’t get a large number of combat casualties today. They’re more likely to have mothers giving birth to babies, and Faison didn’t want his corpsmen changing diapers.
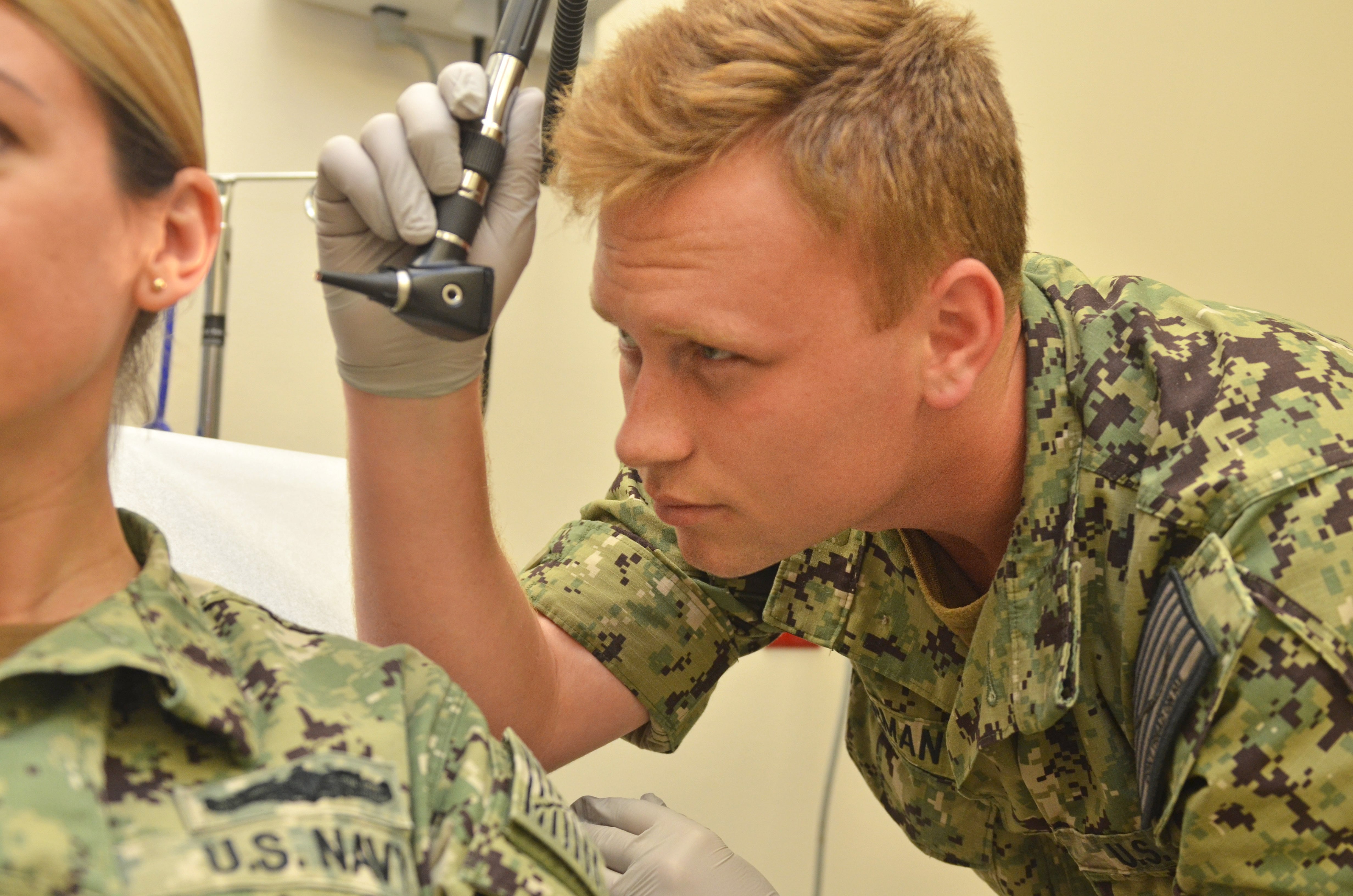
If trauma wouldn’t come to his medical facilities, he’d send corpsmen to emergency rooms in major American cities.
For nearly two decades, the Navy has been sending medical teams to Los Angeles, but Faison’s aides hammered out another deal with a Cleveland hospital. They’ve continued to work on similar initiatives in New York, Seattle and Austin, Texas, too.
Every other month, the Navy sends 30 “A” School grads to Chicago to witness blood and complex patient care so when a sailor or Marine yells “Corpsman up!” they’ll run to the sound of the gunfire and know what to do when they get there.
“They’re so good, when a casualty rolls in the doctors ask for them, not the nurses,” Faison said. “It’s created some drama. We’re working through that.”
Faison sees another payoff with the programs, too — making it easier for patients to connect with Navy medicine.
One of his initiatives — Connected Corpsmen in the Community — kicked off in Florida’s Naval Hospital Pensacola in late 2017.
The Navy’s medical system at home has been centered on large medical hospitals for generations. To get care, a patient was directed to primary care clinics, usually inside or near the hospital, even if they weren’t on the same base as the service member.
In Pensacola, sailors spent long hours commuting to the hospital and then moving through its wards to see physicians, retrieve prescriptions and obtain records.
Although researchers knew that 70 percent of the patients who go to Navy hospitals don’t need to see a physician, sailors, most of them students, were still being sent to the primary care clinics on Pensacola’s medical campus.
So Faison’s teams began moving clinics into the basements of the military schools there and staffing them with newly minted corpsmen. They’re overseen by independent duty corpsmen, with physicians connected by a telemedicine screen if they’re needed.
“We cut absenteeism in schools by 93 percent,” Faison said, a real savings to the Navy.

Part of Faison’s push to get corpsmen into the community also stemmed from the Navy’s need to compete with “minute clinics,” online healthcare services, unregulated cellphone medical apps of dubious accuracy and other 21st century innovations designed to woo patients with convenience.
While they proliferated and Congress offered more choices for military families to find care in town, Faison faced the dilemma of military hospitals becoming irrelevant to a younger generation of sailors.
Fewer patients meant less chances for corpsmen to learn about taking care of the sick and injured. And the inability for government electronic records systems to connect with private sector providers spelled trouble for a service that needs to take the pulse of its personnel.
“The last thing I ever want is a CO to call me and say, ‘Doc, what’s going on with my sailor?’ and I’ve got to say, ‘I don’t know. He’s getting his care somewhere else,’” Faison told Navy Times.
Navy medicine had to reinvent itself, driving costs down and patient outcomes up. Faison’s mantra became “value-based care,” the subject of his speech in Brazil. His Navy got so good at it, Faison found himself moonlighting as an instructor every few months at Harvard Business School, where he taught healthcare executives the lessons his physicians were learning nationwide.
“The first question we ask you is, ‘Hey, what would success be in your treatment?’ And we gear your treatment around what you consider to be a success,” Faison told Navy Times. “What does that mean? You now have skin in the game. What we’ve found is that when you do that, compliance goes up.”
For example, a retired sailor wants to walk his daughter down the aisle at her wedding, without suffering diabetic foot pain. That’s the goal. It’s the Navy’s job to figure out how to help get the patient there.
Sometimes, math and computer science help light a path. About one out of every five residents in San Diego County county qualifies for military healthcare. That’s roughly 250,000 people, but not every patient is the same.
The Navy discovered that 640 beneficiaries — about a quarter of 1 percent of the patient population —accounted for 15 percent of the Navy healthcare system’s costs there.
Because they use so many medical services, they’re nicknamed “hot spotters.” One patient averaged an ER visit daily.
And researchers began to realize that they also used municipal and county services, everything from 911 dispatch, firefighters and paramedics to police officers to connect with healthcare providers.
So Faison’s team targeted 200 of the patients in a program that partnered the Navy with local agencies to share services, such as home healthcare and monitoring equipment and transporting them to scheduled appointments instead of emergency room visits.
That saved the Navy $4 million in the first year, just for 200 people. The second year? $12 million.
“So then we looked at how we could predict who these people were going to be before they became hot spotters, because once they become hot spotters you’re already behind the power curve. They’re using our services.” said Faison.
Researchers developed algorithms to target those patients most likely to suffer complex, serious and expensive ailments, formulas that now are used increasingly across Navy Medicine.

Faison told Navy Times he wished he could’ve stayed a little longer to finish some of the reforms, especially those that leaned on telemedicine.
But after 39 years in uniform, retirement loomed and he had to close what he called “chapter 1” of his life.
He’s going to stay a physician, but he’s eyeing a “leadership in medical education” post somewhere, probably at a university medical school that concentrates on reaching out to underserved minorities.
“You know, you go into medicine to help people,” Faison said. “Chapter 2? I feel like I help people in this job and in my career in the military. Chapter 2 is an extension of that, just in a different way.”
RELATED





